We treat extensive emergencies at our A&Es, which include:
The triage system plays a crucial role in prioritising patients based on the acuity of their clinical presentation.
Upon arrival at the emergency department, the triage nurse will assess your condition and categorise according to the severity of your condition. This assessment ensures that those with critical or urgent medical requirements receive immediate attention and care, allowing us to provide timely and appropriate treatment to all patients.
At our hospitals, we follow the 5-level triaging system, that is:
Critical
(Seen immediately, 0-5
minutes)
Semi-critical / high risk
(Seen within 15 minutes)
Non-Critical
Sub-category G1
(Seen in 30 minutes)
Sub-category G2
(Seen in 60 minutes)
Sub-category G3
(Seen in 90 minutes)
We are committed to optimising efficiency and reducing waiting times for all our patients.
If you encounter any delays, our nurses are always available to help you and make sure that your condition is being monitored.
Knowing basic first aid techniques can make a significant difference in critical situations before professional medical help arrives. It is a vital and fundamental skill that serves as the initial response to injuries, illnesses, and emergencies where timely medical intervention is not readily available.
Administering proper first aid can help prevent the worsening of injuries or conditions. For instance, stop bleeding, immobilising fractures, or clearing airways can prevent complications.
In life-threatening situations, such as cardiac arrest, the timely application of first aid techniques such as cardiopulmonary resuscitation (CPR) can save lives.
To help you feel more prepared in moments like these, we've put together a First Aid E-Book filled with detailed, clear steps you can take while waiting for help to arrive.
The following are some common medical emergencies and what you can do to help while waiting for an ambulance to arrive.

First Aid Measures for Burns and Scalds
What to do if someone has a burn injury?
Step 1: Remove any jewellery or other restrictive garments quickly and gently before the affected area swells up.
Step 2: Hold the affected area under cool, running water for 5 minutes.
Step 3: Alternatively, the wound can be covered with wet gauze or towels for at least 30 minutes.
Step 4: For minor burns and scalds, paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) can be taken for pain relief.
Step 5: Go to the hospital’s Accident & Emergency.
First Aid Measures for Choking
What to do when an adult is choking?
Step 1: Call an ambulance immediately.
Step 2: Encourage the person to cough. However, if choking is severe, they may not be able to breathe, speak or cough.
Step 3: Perform chest blows by standing behind the person. Lean the person slightly forward and give 5 blows to the upper back with the heel of the hand.
Step 4: If the person is still choking, perform abdominal thrust (Heimlich manoeuvre). Wrap your arms around the waist, create a fist with one hand and position it just above the umbilicus (belly button). With your other hand, grip the fist and deliver and inward and upward thrust simultaneously.
Step 5: Continue step 3 and 4 until the choking is relieved or until ambulance arrives. If the person becomes unresponsive, start CPR.
What to do when a child over 1 year old is choking?
Step 1: Call an ambulance immediately. The child may be unable to speak, breathe or cough with sound while clutching their neck or chest.
Step 2: Perform 5 back blows by hitting firmly on the child’s back between the shoulder blades while holding in a head-down position.
Step 3: If the child is still choking, perform 5 abdominal thrusts (Heimlich manoeuvre). Hold the child around the waist and administer an inward and upward thrust simultaneously, just above the umbilicus (belly button).
Step 4: Continue step 2 and 3 until blockage dislodges or ambulance arrives. If the child becomes unresponsive, start CPR.
What to do when an infant is choking?
Step 1: Call an ambulance immediately. Infant may be unable to cry, breathe, cough or make any noise.
Step 2: Perform 5 back blows by holding the infant face-down along your thigh, ensuring that their head is positioned lower than their bottom. Deliver firm blows to their back between the shoulder blades using the heel of your hand.
Step 3: If the infant is still choking, perform 5 chest thrusts. Turn the infant over so they are facing upwards. Position two fingers in the middle of their chest, just below the level of the nipples and push downwards firmly up to 5 times.
Step 4: Continue step 2 and 3 until blockage dislodges or ambulance arrives. If the infant becomes unresponsive, start CPR.
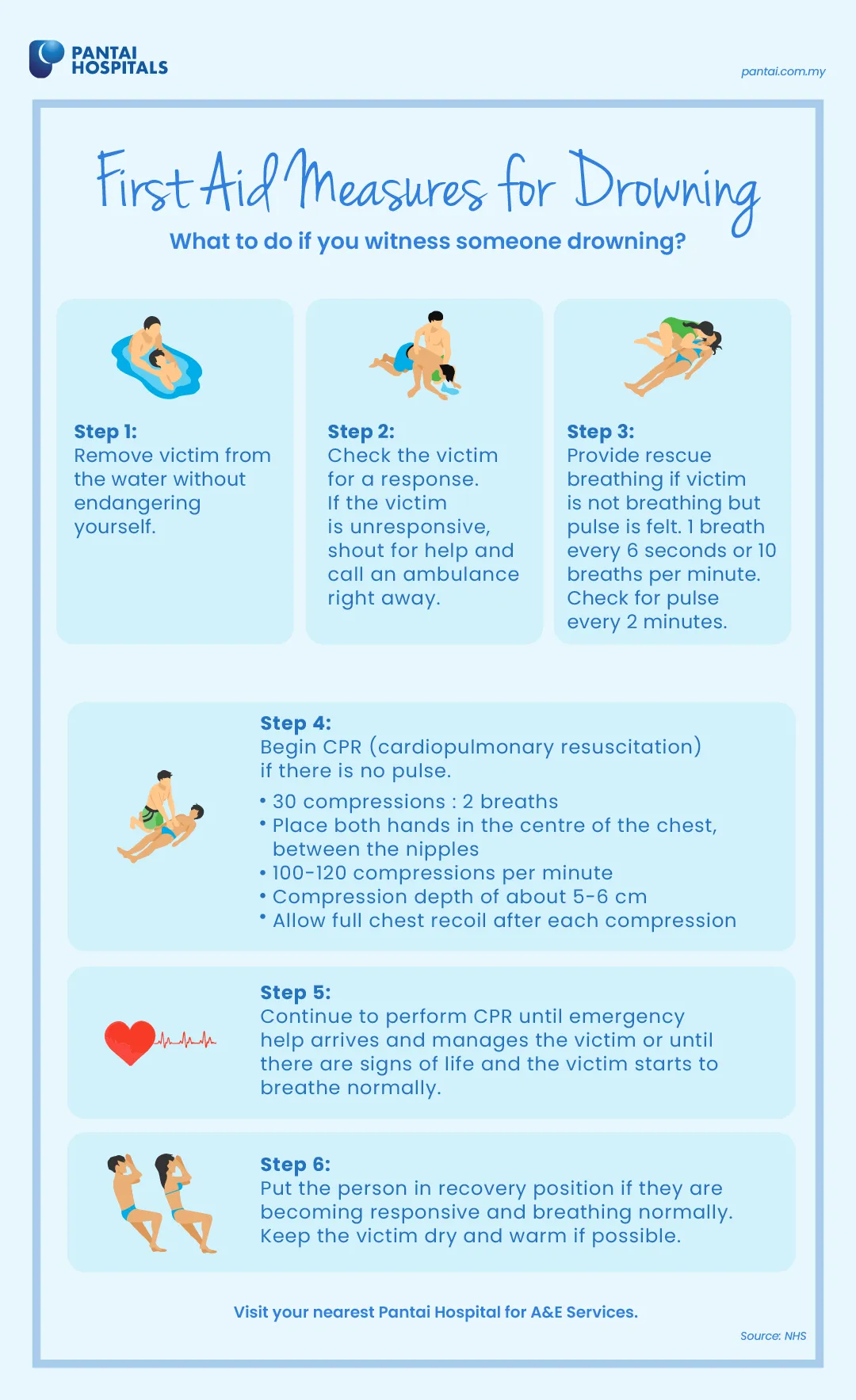
First Aid Measures for Drowning
What to do if witness someone drowning?
Step 1: Remove victim from the water without endangering yourself.
Step 2: Check the victim for a response. If the victim is unresponsive, shout for help and call an ambulance right away.
Step 3: Provide rescue breathing if victim is not breathing but pulse is felt. 1 breath every 6 seconds for 10 breaths per minute. Check for pulse every 2 minutes.
Step 5: Continue to perform CPR until emergency help arrives and manages the victim or until there are signs of life and the victim starts to breathe normally.
Step 6: Put the person in recovery position if they are becoming responsive and breathing normally. Keep the victim dry and warm if possible.
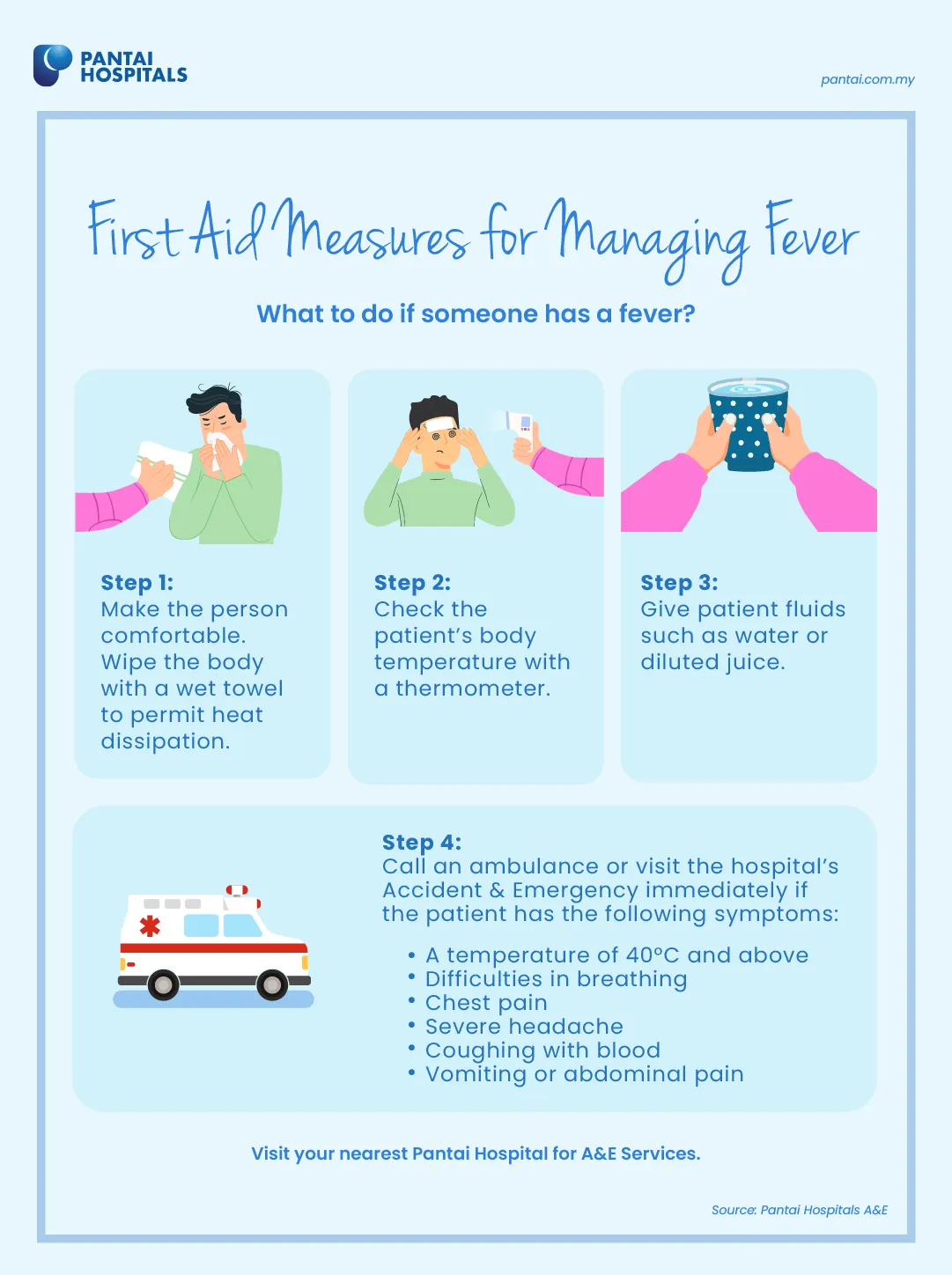
First Aid Measures for Managing Fever
What to do if someone has a fever?
Step 1: Make the person comfortable. Wipe the body with a wet towel to permit heat dissipation.
Step 2: Check the patient’s body temperature with a thermometer.
Step 3: Give patient fluids such as water or diluted juice.
Fever in infants and toddlers
Fever in children (> 2 years old)
There is probably no cause for alarm if your child has a fever but is responsive. This means your child makes eye contact with you and responds to your facial expressions and to your voice. Your child may also be drinking fluids and playing.
Ask your child's healthcare provider for guidance in special circumstances, such as a child with immune system problems or with a pre-existing illness.
Remember: Do not give aspirin to anyone under the age of 16.
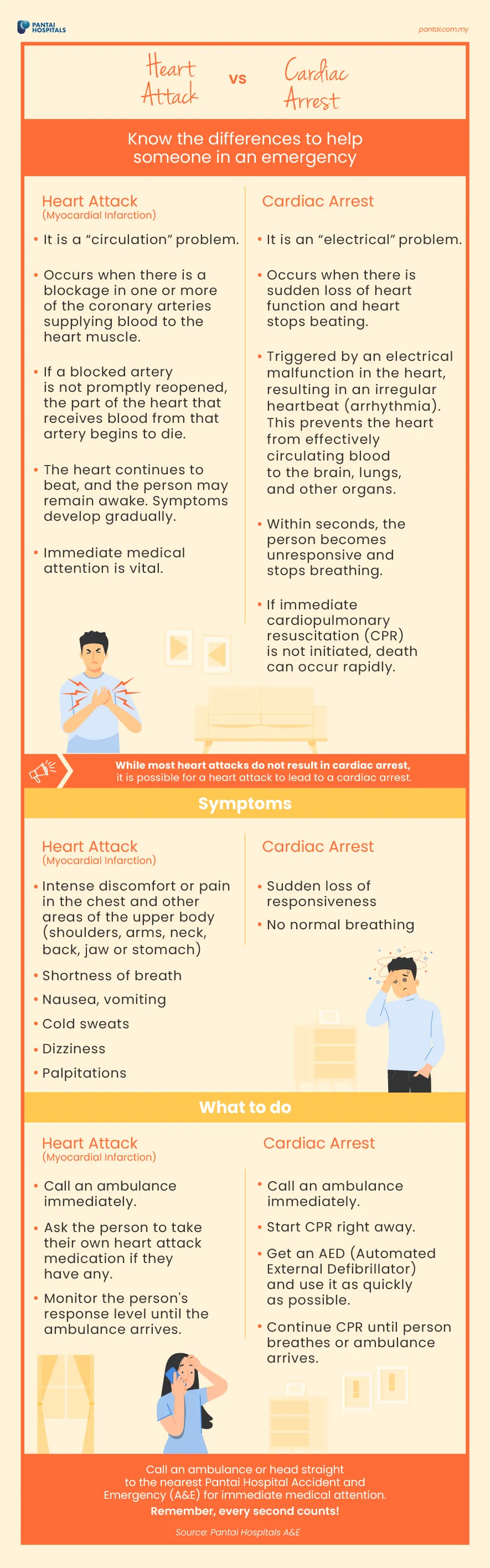
Heart attack vs Cardiac arrest
Know the differences to help someone in an emergency
Heart attack (Myocardial infarction) | Cardiac arrest | |
What is it? |
|
|
While most heart attacks do not result in cardiac arrest, it is possible for a heart attack to lead to a cardiac arrest. | ||
What are the symptoms? |
|
|
What to do? |
|
|
Call an ambulance or head straight to the nearest Pantai Hospital Accident and Emergency (A&E) for immediate medical attention. Remember, every second counts!

First Aid Measures for Poisoning
What to do in case of poisoning?
Step 1: Call an ambulance immediately.
Step 2: Check the scene and person and try to find out what poison was taken.
Step 3: Look for labels on any containers near the victim.
Step 4: Do not give the person anything to eat or drink.
Step 5: Wash your hands immediately if you touch the victim or poison containers nearby to reduce the risk of contamination.
B.E.F.A.S.T to spot a stroke!
How to tell if someone is having a stroke. Look out for the following signs.
Balance |
|
Eyes |
|
Face |
|
Arm |
|
Speech |
|
Time |
|
Call an ambulance or head straight to the nearest Pantai Hospital Accident and Emergency (A&E) for immediate medical attention. Remember, every second counts!

Anaphylaxis (serious allergic reaction)

Asthma Attacks

Upper Gastrointestinal Bleeding