Also known as icterus, jaundice is a medical condition that causes the skin, sclera of the eyes, and mucus membrane to turn yellow.
The term ‘jaundice’ is derived from the French word “jaunisse”, meaning yellow disease. The yellowish discolouration happens due to fluid secreted by the liver, known as bilirubin. It is produced by the normal breakdown of red blood cells in the body. This fluid is metabolised in the liver and excreted as bile from the body.
Jaundice is mainly caused due to the disruption in metabolism, production, or excretion of bile which leads to deposits of excessive amounts of bile in the body.
Similar to what happens in adults, jaundice in a newborn or neonatal jaundice is the yellow appearance in a newborn's skin. This happens when bilirubin builds up in the infant's blood.
During pregnancy, the mother's liver removes bilirubin for the foetus. However, after childbirth, the baby's liver must start to remove bilirubin as there is no further assistance from the mother's body.
It is common for newborns to have jaundice. While most cases are not severe, some newborns may develop pathological jaundice, which is more severe and may be indicative of an underlying medical issue. Hence, it is essential to seek appropriate medical intervention and failure to do so could result in more severe consequences such as brain damage.
Let's look at some common types of jaundice in newborns.
Physiological jaundice is the most common type of jaundice found in newborns and is considered quite normal. It develops on the second or third day after birth. Once the newborn's liver matures, it slowly begins to get rid of excess bilirubin.
Breast milk jaundice usually sets in after the baby's first week of life and takes a month or more to disappear. This is generally due to the presence of a substance in the breast milk, which interferes with the break down and excretion of bilirubin.
Breastfeeding jaundice is quite different from breast milk jaundice. Breastfeeding jaundice occurs when the baby is not getting enough breast milk. This can also happen when the mother does not start to produce enough milk or due to nursing difficulties.
Breastfeeding jaundice usually happens during the first week of delivery and may resolve sooner than breast milk jaundice.
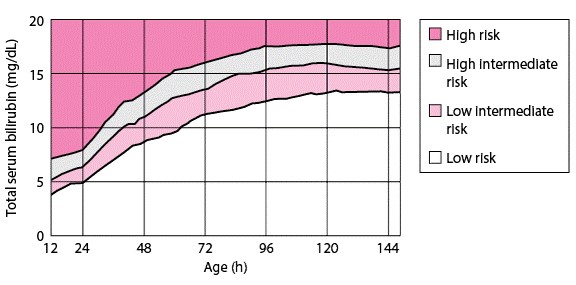
Bilirubin levels are usually highest in the first 3 to 5 days after the baby is born. The doctor will periodically estimate the bilirubin levels in the baby's blood.
Transcutaneous Bilirubinometry is a method using a sensor that measures the bilirubin levels through the baby's skin. If the levels are high, a blood test will be immediately done to confirm the results.
In typical cases, jaundice can appear 2 days after birth and disappear when the baby is about 2 weeks old. If a baby is born prematurely, it may take around 5 to 7 days to appear and disappears in about 3 weeks.
The most visible sign for jaundice is the yellowish appearance of the skin. However, this might sometimes go unnoticed if your baby has a darker skin tone. The discolouration is more noticeable in the head and face. Additionally, you can see that the yellow will intensify if you press that area of skin with your finger.
You may also notice a yellowish tinge:
Other symptoms of jaundice in newborns include:
The following are some factors that can increase the risk of jaundice in a newborn.
As mentioned earlier, in most cases, newborn jaundice disappears as the baby's liver starts its normal function and continues to develop. This typically takes around 2 to 3 weeks.
Feeding your baby around 9 to 11 times a day can help to stimulate bowel movements which will help to get rid of excess bilirubin.
However, if it is a severe form of jaundice, proper medical treatment is essential. One of the effective methods used is phototherapy, where light breaks down the bilirubin in the baby's body.
The baby is placed under specialised blue lights in a nursery or NICU (Neonatal Intensive Care Unit) wearing protective diapers and goggles. In addition, an optical fibre blanket is placed under the baby.
The blue spectrum lights are harmless and give visible results in 2 to 3 days. In some instances, you could provide light therapy at home if your baby's bilirubin levels are not high.
In some rare cases, exchange transfusion is needed if phototherapy fails. This method replaces the baby's blood with healthy donated blood.
If severe neonatal jaundice is left untreated, it may develop into a severe condition known as kernicterus. The excess bilirubin can potentially damage the central nervous system. Additionally, excess bilirubin could cause damage to the spinal cord, and the results could be life-threatening.
Symptoms of kernicterus in newborn babies include:
As kernicterus progresses, additional symptoms occur, such as muscle spasms which causes arching of the body, seizures, etc.
The treatment, in such cases, could include exchange transfusion which should be promptly instituted.
In cases where significant damage to the brain has already occurred prior to treatment, the infant may be at risk of developing additional medical conditions, such as:
Sunlight has a limited role in the treatment of neonatal jaundice. However, studies have shown that sunlight exposure can help reduce jaundice's intensity in mild to moderate cases.
It is also essential to ensure that sunlight exposure is direct and not through any filter. However, this method is not practical for newborns who have severe jaundice.
All newborns are (and should be) examined for jaundice within 72 hours of birth. While most cases of jaundice resolve easily and on their own within a few days, it is important to get early medical intervention.
A dedicated and expert team of paediatricians at Pantai Hospital is available for consultation to provide the best care and assistance. If you notice your newborn having concerning symptoms that point to jaundice, get in touch with us to book an appointment today for a check-up.
Pantai Hospitals have been accredited by the Malaysian Society for Quality in Health (MSQH) for its commitment to patient safety and service quality.